Contraceptive Access
Improving contraceptive access and equity
Our research aims to improve access to contraception while reducing coercion and increasing patient agency through patient-centered approaches to care. We investigate basic needs adversity that stand in the way of access to contraception. We also identify medical barriers that hinder access, and design effective interventions to improve care. Our studies evaluate approaches to expand access to contraception, including
- Raising awareness of contraceptive options, where to find them, and risks and benefits
- Increasing venues to access contraception including the pharmacy and telemedicine
- Training providers to offer high quality, evidence-based counseling and a wide array of methods
- Provision of care in varied practice settings
- Elimination of unnecessary medical exams and visit requirements
As part of the effort to expand access, we have evaluated the provision of contraception in a range of practice settings, including community clinics, pharmacies, primary care, school-based clinics, and abortion providers. We have conducted studies on over-the-counter and direct pharmacy access to emergency contraception, advance provision, and telemedicine access to contraception.
We educate reproductive age populations and providers on new methods, including ones that are especially useful today, such as self-administered Depo-SubQ that does not require clinic visits and Opill® that is available directly at the pharmacy.
We have studied health care providers’ contraceptive education and counseling practices to assess the extent to which they are evidence-based and to identify the need for training on contraceptive eligibility and indications.
Our research has also focused on streamlining access to reproductive health care and reducing unnecessary medical tests, including removing the pelvic exam requirement for hormonal contraception. The pelvic examination can present an obstacle for patients seeking to prevent pregnancy, especially for adolescents. While the dissemination of new clinical practices can be a lengthy process, our research has helped to move reproductive health care in the direction of greater clinic efficiency and improved patient health outcomes.
Featured Research
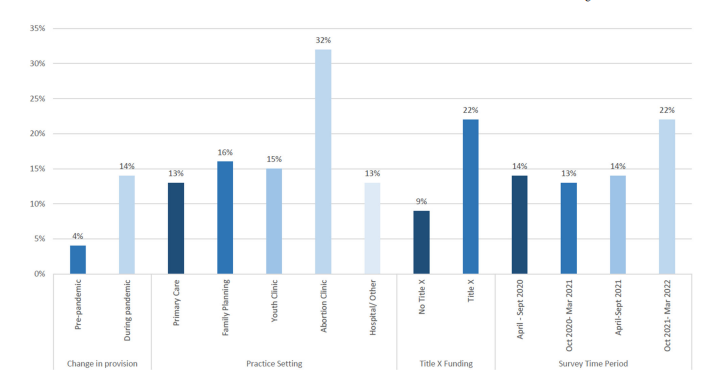
Self-administered Depo-SubQ more available during COVID-19, but overall availability remains low
According to our 2024 study published in Contraception, although self-administered Depo-SubQ increased during the COVID-19 pandemic, the method availability remains persistently low. Depo-SubQ is a lower hormone injectable method that can accessed directly at the pharmacy and administered at home without a clinic visit.
Selected Publications
- Zia Y, Somerson E, Folse C, Alvarez A, Albergate Davis K, Comfort AB, Brown K, Brandi K, Moayedi G, Harper CC. “I am putting my fear on them subconsciously”: a qualitative study of contraceptive care in the context of abortion bans in the U.S. Reprod Health; 21(1):171, 2024.
- Harper CC, Brown K, Shah Arora K. Contraceptive access in the U.S. post-Dobbs. JAMA Internal Medicine, 2024.
- Yarger J, Hopkins K, Elmes S, Rossetto I, Van Liefde D, De La Melena S, Harper CC. Use of telemedicine to obtain contraception among older adolescents and young adults: inequities by health insurance. Contraception, 2024.
- Yarger J, Hopkins K, Elmes S, Rossetto I, De La Melena S, McCulloch CE, White K, Harper CC. Perceived Access to Contraception via Telemedicine Among Young Adults: Inequities by Food and Housing Insecurity. J Gen Intern Med; 38(2):302-308, 2023.
- Hopkins K, Yarger J, Rossetto I, Sanchez A, Brown E, Elmes S, Mantaro T, White K, Harper CC. Use of preferred contraceptive method among young adults in Texas and California: A comparison by state and insurance coverage. PLOS One; 31;18(8):e0290726, 2023.
- Comfort, AB, Alvarez A, Goodman S, Upadhyay U, Mengesha B, Karlin J, Shokat M, Blum M, Harper CC. Provision of DMPA-SC for self-administration in different practice settings during the COVID-19 pandemic: Data from providers across the United States, Contraception, 2023.
- Harper CC, Jones E, Brindis CD, Watson A, Schroeder R, Boyer CB, Edelman A, Trieu S, Yarger J. Educational Intervention among adolescents and young adults on emergency contraception options. Journal of Adolescent Health;72(6):993-996, 2023.
- Yarger JE, Schroeder R, Cabral M, Lamme JS, McCulloch CE, Trieu SL, de Jounge A, Harper CC. An Educational Intervention to Raise Awareness of Contraceptive Options Among Young People. Journal of Women’s Health; 31(2):252-260, 2022.
- Rao L, Comfort AB, Dojiri S, Goodman S, Yarger J, Shah N, Folse C, Blum M, Hankin J, Harper CC. Telehealth for Contraceptive Services During the COVID-19 Pandemic: Provider Perspectives. Women’s Health Issues, 2022.
- Comfort AB, Rao L, Goodman S, Raine-Bennett T, Barney A, Mengesha B, Harper CC. Assessing differences in contraceptive provision through telemedicine among reproductive health providers during the COVID-19 pandemic in the United States. Reprod Health 19(1): 99, 2022.
- Comfort AB, Krezanoski P, Rao L, El Ayadi A, Tsai A, Goodman S, Harper CC. Mental health among outpatient reproductive health care providers during the US COVID-19 epidemic. Reproductive Health; 18(1):49, 2021.
- Yarger J, Schroeder R, Blum M, Cabral M, Perelli B, Harper CC. Concerns about the Cost of Contraception among Young Women Attending Community College. Women’s Health Issues; S1049-3867(21)00028-1, 2021. (Editor’s Choice Article for Sept/Oct 2021 issue).
- Holt HK, Sawaya GF, El Ayadi AM, Henderson JT, Rocca CH, Westhoff CL, Harper CC. Delays in clinic visits for contraception due to concerns regarding pelvic examination among women with history of intimate partner violence. Journal of General Internal Medicine; 36(7): 1883-1889, 2021.
- Rocca CH, Goodman S, Grossman DJ, Cadwallader K, Thompson KM, Talmont E, Speidel JJ, Harper CC. Contraception after medication abortion in the United States: results from a cluster randomized trial. American Journal of Obstetrics and Gynecology 218(1):107e.1-8, 2018.
- Rocca CH, Thompson KM, Goodman S, Westhoff CL, Harper CC. Funding policies and postabortion long-acting reversible contraception: results from a cluster randomized trial. American Journal of Obstetrics and Gynecology 214(6):716.e1-8, 2016.
- Gibbs SE, Rocca CH, Bednarek P, Thompson KM, Darney PD, Harper CC. Long-acting reversible contraception counseling and use for older adolescents and nulliparous women. Journal of Adolescent Health 59(6):703-709, 2016.
- Hsu A, Henderson JT, Harper CC, Sawaya GF. Obstetrician–gynecologist practices and beliefs regarding external genitalia inspection and speculum examinations in healthy older asymptomatic women. Journal of the American Geriatrics Society 64(2): 293-8, 2016.
- Rafie S, Kelly S, Gray EK, Wong M, Gibbs S, Harper CC. Provider opinions regarding expanding access to hormonal contraception in pharmacies. Contraception 26(2):153-160, 2016.
- Biggs A, Harper CC, Brindis C. California Family Planning Health Care Providers’ Challenges to Same-Day Long-Acting Reversible Contraception Provision. Obstetrics & Gynecology 126(2):338-45, 2015.
- Schneider A, Henderson JT, Harper CC, Hsu A, Saraiya M, Sawaya GF. Obstetrician-gynecologists’ beliefs about performing less cervical cancer screening: the pendulum swings. American Journal of Obstetrics & Gynecology pii: S0002-9378(15)00719-X, 2015.
- Henderson, JT, Yu JM, Harper CC, Sawaya GF. U.S. clinicians’ perspectives on less frequent routine gynecologic examinations. Preventive Medicine 62;49-53, 2014.
- Yu JM, Henderson JT, Harper CC, Sawaya GF. Obstetrician-gynecologists’ beliefs on the importance of pelvic examinations in assessing hormonal contraception eligibility. Contraception90(6):612-4, 2014.
- Thompson KMJ, Stern L, Gelt M, Speidel JJ, Harper CC. Counseling for IUDs & implants: Are health educators & clinicians on the same page? Perspectives on Sexual and Reproductive Health 45:191-195, 2013.
- Harper CC, Stratton L, Raine TR, Thompson K, Henderson JT, Blum M, Postlethwaite D, Speidel JJ. Counseling and provision of long-acting reversible contraception in the US: National survey of nurse practitioners. Preventive Medicine 57:883-8, 2013.
- Henderson JT, Saraiya M, Martinez G, Harper CC, Sawaya G. Changes to cervical cancer prevention guidelines: Effects on screening among U.S. women ages 15-29. Preventive Medicine 56:25-9, 2013.
- Henderson JT, Harper CC, Gutin S, Saraiya M, Chapman J, Sawaya G. Routine bimanual pelvic examinations: Practices and beliefs of US obstetrician-gynecologists. American Journal of Obstetrics & Gynecology 208:709e1-7, 2013.
- Thompson KMJ, Raine TR, Foster DG, Speidel JJ, Darney PD, Brindis CD, Harper CC. Access to levonorgestrel emergency contraception: Science v. federal politics. Women’s Health 9:139-43, 2013.
- Rafie S, Haycock M, Rafie S, Yen S, Harper CC. Direct pharmacy access to hormonal contraception: California physician and advanced practice clinician views. Contraception 86:687-93, 2012.
- Morse J, Freedman L, Speidel JJ, Thompson KMJ, Stratton L, Harper CC. Post-abortion contraception: Qualitative interviews on counseling and provision of long-acting reversible contraceptive methods. Perspectives on Sexual and Reproductive Health 44:100-106, 2012.
- Thompson KMJ, Speidel JJ, Saporta V, Waxman NJ, Harper CC. Contraceptive policies affect post-abortion provision of long-acting reversible contraception. Contraception 83:41-47, 2011.
- Harper CC, Henderson JT, Schalet A, Becker D, Stratton L, Raine TR. Abstinence and teens: Prevention counseling practices of health care providers serving high-risk patients in the United States. Perspectives on Sexual and Reproductive Health 42:125-132, 2010.
- Stotland NE, Gilbert P, Bogetz A, Harper CC, Abrams B, Gerbert B. Preventing excessive weight gain in pregnancy: How do prenatal care providers approach counseling? Journal of Women’s Health 19:807-814, 2010.
- Henderson JT, Sawaya GF, Blum M, Stratton L, Harper CC. Pelvic examinations and access to oral hormonal contraception: Results from a national survey. Obstetrics & Gynecology 116:1257-64, 2010.
- Goodman S, Hendlish SK, Benedict C, Reeves MF, Pera-Floyd M, Foster-Rosales A. Increasing intrauterine contraception use by reducing barriers to post-abortal and interval insertion. Contraception 78(2):136-42, 2008.
- Goodman S, Hednlish SK, Reeves, MF, Foster-Rosales, A. Impact of immediate postabortal insertion of intrauterine contraception on repeat abortion. Contraception 78(2):143-8, 2008.
- Harper CC, Weiss DC, Speidel JJ, Raine-Bennett T. Over the counter access to emergency contraception for teens. Contraception 77:230-233, 2008.
- El-Ibiary SY, Raine T, McIntosh J, Darney PD, Harper CC. Pharmacy access to emergency contraception: the perspective of pharmacists at a chain pharmacy in San Francisco, California. Journal of the American Pharmacists Association 47:702-710, 2007.
- Polis CB, Schaffer K, Blanchard K, Glasier A, Harper CC, Grimes DA. Advance provision of emergency contraception for pregnancy prevention: a meta analysis. Obstetrics & Gynecology 110:1379-88, 2007.
- Polis CB, Schaffer K, Blanchard K, Glasier A, Harper CC, Grimes DA. Advance provision of emergency contraception for pregnancy prevention (full review). Cochrane Database of Systematic Reviews, 2007.
- Raine TR, Harper CC, Rocca CH, Fisher R, Padian N, Klausner JD, Darney PD. Direct access to emergency contraception through pharmacies and effect on unintended pregnancy and STIs: A randomized, controlled trial. JAMA 293:54-62, 2005.
- Raine T, Marcel AV, Rocca CH, Harper CC. The other half of the equation: Serving young males within a young women’s reproductive health clinic. Perspectives on Sexual and Reproductive Health 35(5):208-214, 2003.
- Stewart FH, Harper CC, Ellertson CE, Grimes DA, Sawaya GF, Trussell J. Clinical Breast and Pelvic Examination Requirements for Hormonal Contraception: Current Practice vs Evidence . JAMA 285(17):2232-2239, 2001.
- Harper C, Balistreri E, Boggess J, Leon K, Darney P. Provision of hormonal contraception without a mandatory pelvic exam: “First Stop,” a California demonstration project. Family Planning Perspectives 33(1):13-18, 2001.
- Sawaya GF, Harper C, Balistreri E, Boggess J, Darney P. Cervical neoplasia risk in women provided hormonal contraception without a Pap smear. Contraception 63(2):57-60, 2001.